Skeletal muscle relaxants
Introduction
Most of the time, physiotherapist come across skeletal muscle relaxants during their practice. Knowing about skeletal muscle relaxants (especially centrally acting skeletal muscle relaxants) helps in rehabilitation processes. There are two types of muscle relaxants, first one is peripherally acting skeletal muscle relaxant and second one is centrally acting muscle relaxants. As a physiotherapist, we might have seen centrally acting muscle relaxants. Because, centrally acting drugs are prescribed for muscle spasms in acute pain conditions and spasticity in neurological conditions (e.g. stroke, parkinsonism, spinal cord injury). Rather, peripherally acting drugs are not known drugs by physiotherapists. Because, peripherally acting muscle relaxants are used during surgical procedures.
Classification

Peripherally acting agents
These drugs act on neuromuscular junction or directly on the muscles. based on its action, these drugs are divided into:
- Neuromuscular blocking agents
- Directly acting agents
1. Neuromuscular blocking agents
Neuromuscular blocking agent binds with nicotinic receptor (ach receptor) in post-synaptic membrane of Neuromuscular junction and blocks endplate potential in the muscles. These drugs are again divided into:
A. Non-depolarizing neuromuscular blocker
B. Depolarizing neuromuscular blocker
A. Non-depolarizing neuromuscular blockers
These type of drugs also called as competitive NM blockers. Because, it compete with acetylcholine for binding nicotinic receptor. Once it binds with nicotinic receptor, it will not produce any intrinsic effect on the receptor and also it blocks ach to bind the receptor.
- Short acting:
- Mivacurium Intermediate:
- Vecuronium
- Atracurium
- Cisatracurium
- Rocuronium
- Rapacuronium Long acting:
- D-Tubocurarine
- Pancuronium
- Doxacurium
- pipecuronium
B. Depolarizing neuromuscular blockers
It binds with nicotinic receptor in post synaptic membrane and produces fasciculations and twitches initially. It keeps the membrane potential above the threshold level.
- Succinylcholine
- Decamethonium
2. Directly acting agents
Directly acting agents (e.g. Dantrolene sodium) act directly on the muscle especially on RYR1 receptors in sarcoplasmic reticulum. This type of drugs block calcium induced calcium release from sarcoplasmic reticulum by blocking ryr-1 receptors. As calcium is necessory for actin myosin binding, this agents block calcium release from sarcoplasmic reticulum to reduce or inhibit muscle contraction
Centrally acting agents
These are drugs which reduce skeletal muscle tone by a selective action in the cerebrospinal axis, without altering consciousness. They selectively depress spinal and supraspinal polysynaptic reflexes involved in the regulation of muscle tone without significantly affecting monosynaptically mediated stretch reflex. These drugs act only on CNS (brain and spinal cord). It is classified into three groups:
- Antispasmotic benzodiazepines
- Antispasmotic non-benzodiazepines
- Antispastic drugs
1. Antispasmotic benzodiazepines
Benzodiazepines are commonly used in treatment of anxiety disorder and epilepsy. There are many different benzodiazepines such as alprazolam, bromazepam, diazepam etc... Diazepam is the frquently prescribed drug for muscle spasms and pain. Other benzodiazepines have not been proven superior than diazepam. Effect of this drug results in enhancement of GABA mediated presynaptic inhibition at supraspinal and spinal level. Diazepam is superior to placebo but it is not superior than othen centrally acting relaxants.
Mechanism of action of diazepam: It acts on GABA-a receptor and allow influx of chloride. Which causes hyperpolarization of neurons. So further action potential will not be initiated.
Diazepam is highly lipid soluble and well absorbed from GI tract, metabolized in liver and excreted through kidney. high lipid solubility allows diazepam to crosses the blood brain barrier. Plasma half life of diazepam is 20-50hours. Diazepam is available in 2mg, 5mg and 10mg tablets.
Diazepam and other benzodiazepines have withdrawal symptoms after sudden cessation. It has some adverse effects of impairment of psychomotor performance, cognitive dysfunction, confusion, dizziness and behavioral changes.
2. Antispasmotic non-benzodiazepines
CyclobenzoprineMechanism of action of cyclobenzoprine is unclear. but it produce its action on brainstem. Its onset of action is within 1hour and it has plasma half life of 1-3 days. Cyclobenzoprine is available as 10mg tablets.
ChlorzoxazoneExact mechanism of action is not clear. evidences suggest that it may produce action on spinal and subcortical region. It has plasma half life 1 to 2 hours.
MephenesinIt was the first drug found to cause muscle relaxation in animals without producing unconsciousness and was called internuncial neurone blocking agent because its primary site of action is the spinal internuncial neurone which modulates reflexes maintaining muscle tone. It is not used clinically because orally it causes marked gastric irritation, and injected i.v., it causes thrombophlebitis, haemolysis and fall in BP. It has been included in counterirritant ointments (MEDICREME, RELAXYL) where its irritant rather than muscle relaxant property could be affording relief.
MethocarbamolIt is less sedative and longer acting than mephenesin. Orally it has been used in reflex muscle spasms and chronic neurological diseases. It can be injected i.v. without producing thrombophlebitis and haemolysis— used for orthopedic procedures and tetanus.Studies have postulated that it inhibits acetylcholinesterase. commonly used with pain medications. it has plasma half life of 1 to 2 hours.
TizanidineThis clonidine congener is a central α2 adrenergic agonist, it inhibits release of excitatory amino acids in the spinal interneurones. It may facilitate the inhibitory transmitter glycine as well. Polysynaptic reflexes are inhibited resulting in decreased muscle tone and frequency of muscle spasms without reducing muscle strength.
Efficacy similar to baclofen or diazepam has been noted in multiple sclerosis, spinal injury and stroke, with fewer side effects. Tizanidine is absorbed orally, undergoes first pass metabolism and is excreted by the kidney; t½ 2–3 hours. It is indicated in spasticity due to neurological disorders and in painful muscle spasms of spinal origin.
3. Antispastic drugs
Baclofen is most commonly used drug in spastic conditions. it causes neuronal inhibition through stimulation GABA-b receptors (G-protein coupled receptor). The primary site of action of baclofen is considered to be in the spinal cord where it depresses both polysynaptic and monosynaptic reflexes. It does produce muscle weakness, but is less sedative than diazepam. Spasticity in many neurological disorders like multiple sclerosis, amyotropic lateral sclerosis (ALS), spinal injuries and flexor spasms is reduced, and baclofen is the preferred drug for symptomatic relief.
Baclofen is well absorbed orally and is primarily excreted unchanged in urine with a t½ of 3–4 hours.
Uses of Centrally acting agents
- Acute muscle spasms
- Anxiety
- Spastic neurological disorders
- Tetanus
- Orthopedic manipulations
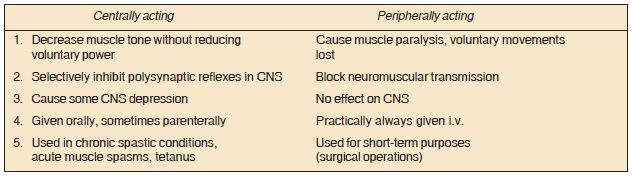
Difference between peripheral and central agents
SHARE:


- Howard J. Waldman, MD., Centrally Acting Skeletal Muscle Relaxants and Associated Drugs (1994).
- Bethan L Richards, Samuel L Whittle, Rachelle Buchbinder., Muscle relaxants for pain management in rheumatoid arthritis (2012).
- M Roussan, C Terrence, G Fromm.,Baclofen versus diazepam for the treatment of spasticity and long-term follow-up of baclofen therapy (1985).
| Name | : | Deva senathipathi |
| Qualifications | : | Physiotherapist |





