Acute Inflammation
Inflammation is defined as local response of living tissue to injury from causative agents. Acute inflammation is the short duration and resolved by complete healing. If acute inflammation persists for longer duration is called chronic inflammation (because of failed healing response). Inflammation is the body defense reaction against causative agents.
Following are the agents which may causes inflammation:
- Infective agents (e.g. bacteria and viruses)
- Immunological agents (e.g. antigen antibody reaction)
- Physical agents (e.g. heat, cold, radiation and mechanical trauma)
- Chemical agents (e.g. organic and inorganic poisoning)
- Inert materials (e.g. foreign bodies)
Physical therapist most often deals with physical agents like mechanical trauma. Heat and cold injuries are common environment related conditions often treated in sports medicine. Inflammation is distinct from infection; it is protective response of the body to causative agents. Sometimes, inflammation can causes damages to the body e.g. anaphylactic reactions of rheumatoid arthritis, insect bites, toxins, drugs.
Signs of acute inflammation
There are 5 cardinal signs of inflammation
- Redness (rubor)
- Swelling (tumor)
- Heat (calor)
- Pain (dolor)
- Loss of function
VASCULAR EVENTS
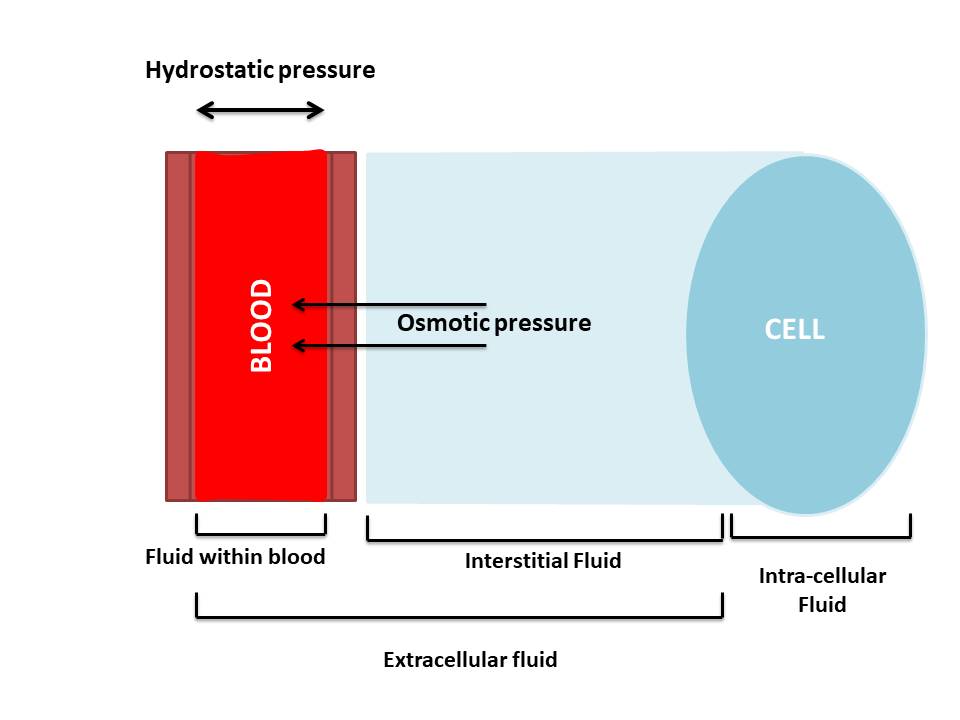
`Vascular event includes changes in hemodynamics and vascular permeability. Before discuss about vascular changes, we need to know about pressures acting within and outside of the blood vessels. There are two types of pressures (hydrostatic pressure and osmotic pressure) which maintain fluid dynamics in and out of blood vessels.
- Hydrostatic pressure: outward forces exerted by fluids inside the blood vessels.
- Osmotic pressure: simple words, it is the force which prevents fluid movement across blood vessel and tissue membrane. Albumin is the blood protein which holds plasma fluids within the blood. Thus, albumin maintains osmotic pressure within the blood vessels.
Hemodynamic changes
|
Followed by persistent vasodilatation (Starts within 30mins of injury)
|
Increased hydrostatic pressure (Transudation of fluid into interstitial space)
|
Slowing or stasis of blood (Increases RBC and leukocytes)
Changes in vascular permeability
In and around injured tissue, there will be accumulation of exudates from vessels. Leakage of fluid from capillaries is due to increased permeability of capillary walls.
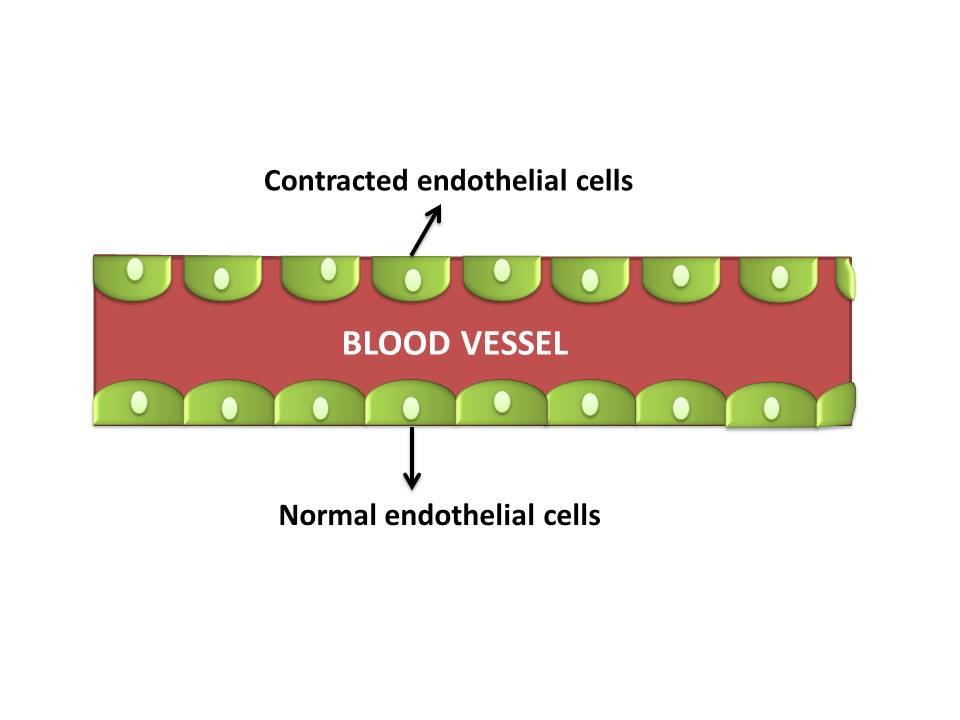
- Following patterns can increase vascular permeability:
- Contraction of endothelial cells
- Direct injury to the endothelial cells
- Leukocyte mediated endothelial damage
- Leakiness in neovascularisation
CELLULAR EVENTS
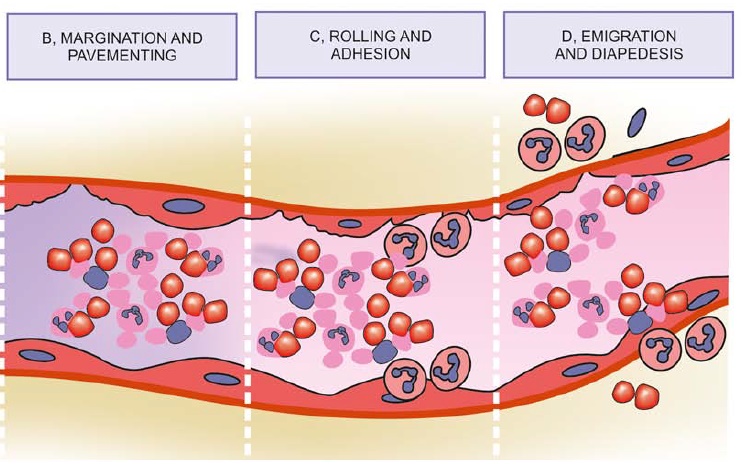
Exudation of leukocytes
Neutrophils are primary cell present during first 24hours after injury. Macrophages are dominant during 24 to 48 hours.
- Margination of leukocytes
- Rolling and Adhesion
- Emigration and Diapedesis
Phagocytosis
Neutrophils and macrophages are involved in phagocytic process. Phagocytosis is defined as process of engulfing of solid particles. It includes foreign bodies, damaged cells or microbial agents.
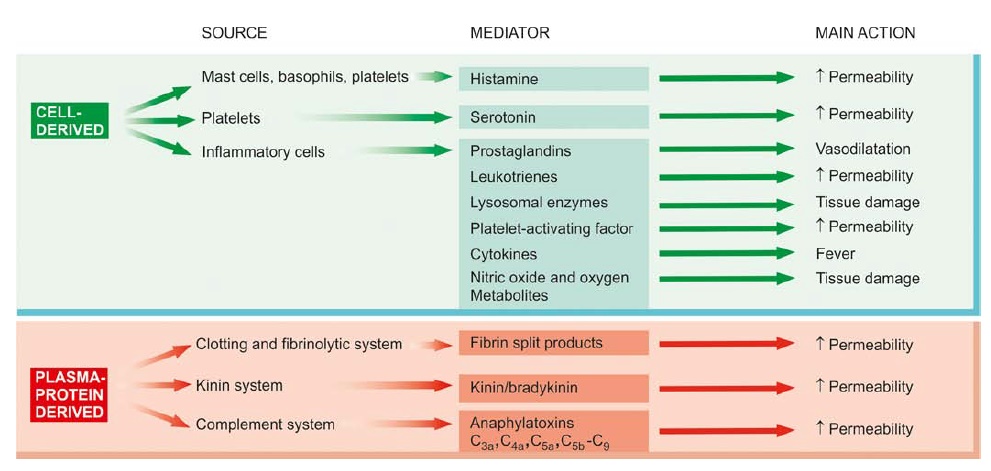
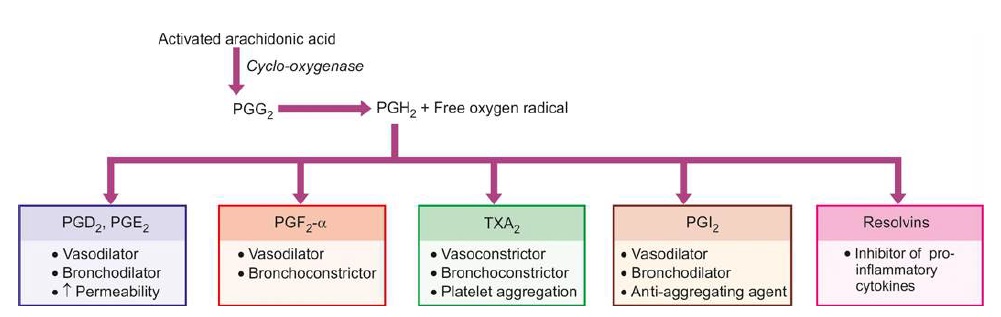
CHEMICAL MEDIATORS OF INFLAMMATION
SHARE:


- Harsh mohan., General pathology.
- Catherine cavellaro goodman., pathological implications for physiotherapist, fourth edition.
- Carine Smith, Maritza J Kruger, Robert M Smith, Kathryn H Myburgh., The inflammatory response to skeletal muscle injury: illuminating complexities (2008).
| Name | : | Deva senathipathi |
| Qualifications | : | Physiotherapist |





