Ischemic Compression Technique
Ischemic compression is a manual technique in which the therapist applies pressure directly over the trigger point. This ischemic compression technique involves the application of sustained pressure for a long enough time to inactivate the trigger points. Travell and Simons termed this therapy 'ischemic compression.' This technique is similar to the Nimmo technique in chiropractic.
On the release of pressure, the skin shows reactive hyperemia. These changes correspond to circulatory changes in the underlying muscle, which is subjected to the same ischemic compression pressure.
Pressure during ischemic compression can be applied with the thumb, finger, knuckle, or elbow depending on the size, depth, and thickness of the muscle being compressed. Specific pressure is applied directly to the center of the trigger point to the patient's tolerance. Care must be taken not to exceed the patient's tolerance, and if the patient tenses or pulls away, then lighter ischemic compression pressure should be applied.
Procedure
- Identify the trigger point.
- Apply perpendicular pressure (ischemic compression) over the trigger point.
- The patient usually feels tenderness, but it should not exceed 7 on the NPRS (Numeric Pain Rating Scale).
- Pressure should be sustained for 15-30 seconds until the pain reduces.
- Increase ischemic compression pressure gradually once the patient feels a reduction in pain.
- Continue this process for 2-3 minutes until the trigger point completely melts away.
Treatment Duration
- 10-30 seconds of sustained ischemic compression pressure
- Gradual increase in pressure for 2-3 minutes until the trigger point completely melts away
- 2-3 sessions per week for several weeks

What is a Myofascial Trigger Point?
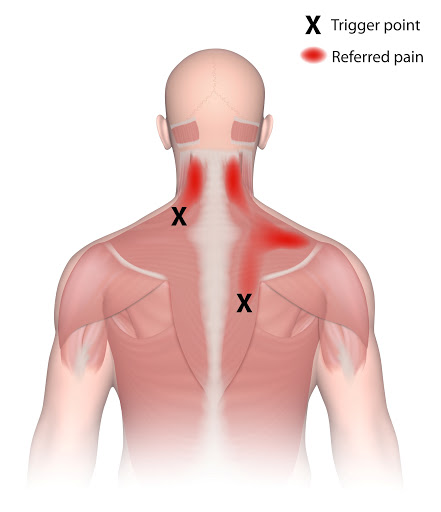
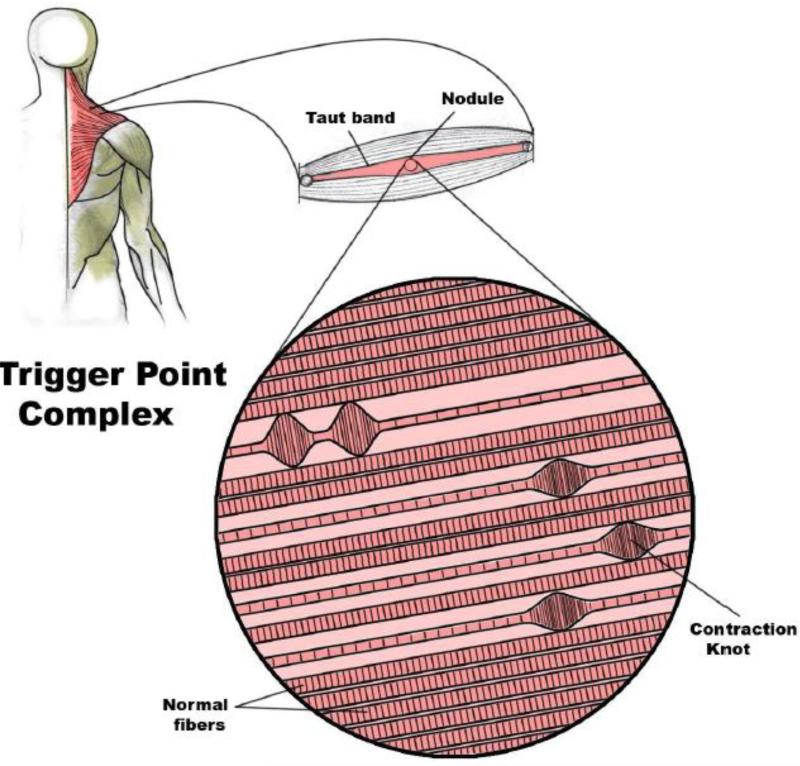
Trigger points are discrete, focal, hyperirritable spots located in a taut band of skeletal muscle. They produce pain locally or at distant sites (referred pattern).
Historical Names
Nodular tumors - Balfour (1816)
Muskelshwiele (muscle collus) - Froriep (1843)
Fibrositis - Gowers (1904)
Myogeloses (muscle colloid) - Schade (1919)
Myofascial Trigger Points - Travell & Rinzler (1950s)
Types of Trigger Points
1. Active Trigger Point (Primary TrPnt)
The reason for presenting complaint. Presence of spontaneous pain and referred pain pattern.
2. Latent Trigger Point
Precursors to active triggers. There is no spontaneous pain; pain and referral patterns are elicited by pressing over the trigger point.
3. Attachment Trigger Point (Enthesis)
Presence of a trigger point at the tendon-osseous junction. Usually present in chronic tendinopathy.
4. Central Trigger Point
The most common trigger point, present at the center of the muscle or in the muscle belly.
5. Satellite Trigger Point
Secondary trigger points formed in the areas of referred pain from the primary trigger point.
6. Diffuse Trigger Point
Multiple satellite trigger points commonly present in scoliosis.
7. Ligament Trigger Point
Studies have shown that trigger points can form in ligaments (Hackett 1958).
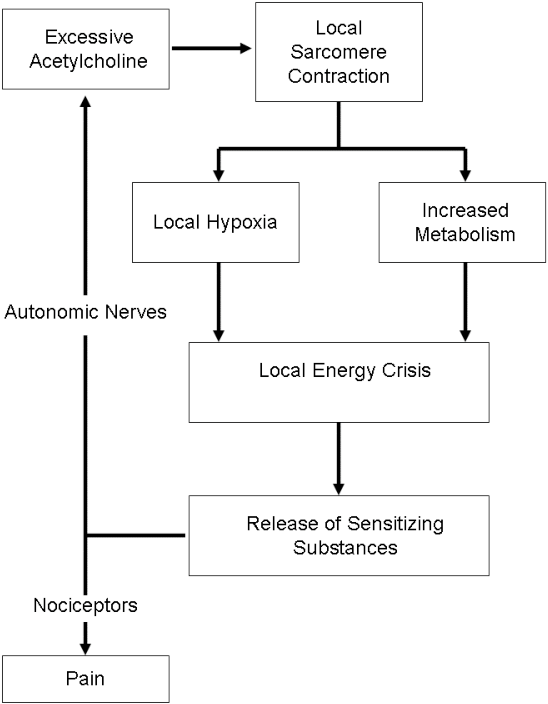
Trigger Point Hypothesis
Recommended Treatment
Following treatment combinations can be used to treat trigger points with ischemic compression technique:
- Myofascial release therapy followed by ischemic compression technique
- Ischemic compression technique + ultrasound
- Ischemic compression technique followed by cryotherapy





